lungs feel like they are burning after covid
 Its also important to stay hydrated with three to four liters a day of fluid (unless you have heart failure) while avoiding alcohol and caffeine and modestly increasing salt intake (unless you have high blood pressure). swollen ankles and feet. It is a strange experience to have to relearn how to do a thing that you never had to learn in the first place. Three things that impact how well (and how quickly) your lungs will heal are: 1. You also have the option to opt-out of these cookies. Web524 Likes, 34 Comments - Lizzie Morse (@lizzies.reading.recs) on Instagram: " . Houston Methodist, Houston, TX. When those exercises can be completed without struggle for a few weeks, they can increase the intensity incrementally until they've reached normal intensity levels.
Its also important to stay hydrated with three to four liters a day of fluid (unless you have heart failure) while avoiding alcohol and caffeine and modestly increasing salt intake (unless you have high blood pressure). swollen ankles and feet. It is a strange experience to have to relearn how to do a thing that you never had to learn in the first place. Three things that impact how well (and how quickly) your lungs will heal are: 1. You also have the option to opt-out of these cookies. Web524 Likes, 34 Comments - Lizzie Morse (@lizzies.reading.recs) on Instagram: " . Houston Methodist, Houston, TX. When those exercises can be completed without struggle for a few weeks, they can increase the intensity incrementally until they've reached normal intensity levels.
Sore throat. Perfect E Learn is committed to impart quality education through online mode of learning the future of education across the globe in an international perspective. COVID-19 is an upper respiratory illness that spreads as an infected person breathes, speaks, clears their throat, or coughs near others even if they don't know they're infected. COVID-19 has been linked to symptoms like throat pain and acid reflux.
If you had severe COVID-19, you might need to work with a respiratory therapist to rebuild your lung function safely. Altman emphasized that younger people who are healthy are at lower risk of developing severe complications after COVID. "If you're in the 9599% range, it's fairly safe to assume that you can try to build your fitness levels back to normal.". Had a great experience here.
Around this time the media started reporting on long haul cases of the virus.
I was not really coughing I would give a pathetic little single cough once or twice a day, and my chest was not feeling congested, there was no phlegm to be cleared.
But opting out of some of these cookies may affect your browsing experience.
COVID-19 might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms.
They also recommend developing strategies to help patients return to activity gradually; conserve their energy; eat healthy foods; stay hydrated; and follow, if necessary, a regimen of medications and herbal and vitamin supplements. Keep your shoulders relaxed.
Frese recommends three exercises that can help you locate and target the muscles that support lung function.
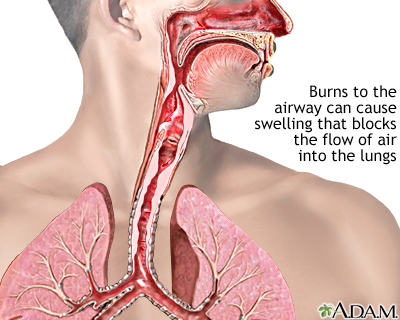
Coronavirus COVID-19 reducing of risk of spreading the infection by covering nose and mouth when coughing and sneezing with tissue or flexed elbow. program which is essential for my career growth. Dr. Connolly: Once in the chest, the virus begins to impact a person's airways causing inflammation.
We use cookies to make interactions with our website easy and meaningful. But COVID-19 can cause symptoms you may not expect, including: Digestive symptoms. These individuals are the victims of long COVID, defined by the CDC as conditions patients experience four or more weeks after recovering from a COVID-19 infection. Many recover initially from COVID-19 only to suffer weeks later from sometimes confounding symptoms that can affect all parts of the body. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Medical researchers have a long way to go too.
Time was a blur. This condition shows up as scarring in the lungs.
Then again, I thought to myself, I am always tired at this time of year. WebIn most cases, lung problems from COVID-19 are reversible. By Rachel Murphy While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe. Experiencing throat and chest burning together can be a symptom of COVID-19. Weve seen patients across the board, Altman said. I drank a lot of fresh ginger tea. By late March all I could do was lie in bed, nap, read and eat.
Australia's Covid-19 face mask advice: can I reuse them, what's the best to use and where to buy? Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion.
Altman noted that the heart has receptors ACE2 (angiotensin-converting enzyme 2) to which the SARS-CoV-2 protein binds.
Web524 Likes, 34 Comments - Lizzie Morse (@lizzies.reading.recs) on Instagram: " . These patients are at a higher risk of hospitalization, persistent illness and potentially death. Altman added that people with a preexisting heart condition heart failure and coronary artery disease, for example generally have a rough course of recovery from COVID-19 and can be at greater risk for lung disease, blood clots and heart attacks. finding exercise more difficult than usual or impossible.
Pursed-lip breathing helps slow your breathing and increases the amount of air that you breathe out, which can help decrease the feeling of breathlessness. We arent entirely sure why it happens, she said. Breathe out through your mouth after each breath that you take in.
In fact, Han says that the lungs are not muscles and therefore cannot be strengthened. I was just too tired. That may be an easier way for the virus to get into the heart muscle, Altman said. To begin, locate and focus on your thoracic diaphragm (the large muscle wall that separates your thoracic cavity from your abdomen). They therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID Clinic. A good way to start is with recumbent biking and rowing, which helps to exercise the heart while reducing strain on the joints and muscles. I was still able to deliver a two-hour lecture, ride my bike, talk to people in meetings, walk to the supermarket; but I was a bit more tired at the end of the day. I had burning lungs, exhaustion and shallow breathing for a total of six weeks.
One major lesson: long COVID is consistently inconsistent. Air sacs in the lungs fill with fluid, limiting their ability to take in oxygen and causing shortness of breath, cough and other symptoms. The lungs are not muscles and cannot be "exercised," but there are ways to strengthen your lungs' support systems if they have been weakened by COVID-19.
It can be 14 days before you realize you have been infected and experience early symptoms such as a fever, sore throat or dry cough. If you had a milder infection, targeting the muscles that support your lungs is a great place to start and these exercises can be done at home. If you had a mild case of COVID-19 with symptoms like a dry cough, sore throat and sometimes a mild case of pneumonia you probably wont have lasting damage.  "What allows the lungs to open is the diaphragm, which sits underneath the lungs. As July begins, I am almost able to breathe normally, but only when I give it my full attention.
"What allows the lungs to open is the diaphragm, which sits underneath the lungs. As July begins, I am almost able to breathe normally, but only when I give it my full attention.
Digestive symptoms sometimes develop before a fever and respiratory symptoms. What Experts Say About Learning to Breathe Again After COVID. These are the patients who can really benefit from seeing us in the multidisciplinary clinic. I could still walk to the shop and carry my shopping home then, a 20-minute walk each way. We still don't fully understand why people with preexisting lung conditions don't make up a larger majority of current COVID-19 cases as initially anticipated. These cookies will be stored in your browser only with your consent. I walked to the clinic very slowly. I realised I was doing something I came to think of as Covid breathing. Try breathing out while holding a tissue in front of your mouth and have the tissue move slightly to provide a helpful visual. Symptoms can range from mild, such as cough, shortness of breath and fevers, to critical disease, including respiratory failure, shock and multi-organ system failure.
They think I have Covid-19, I said. Perfect E learn helped me a lot and I would strongly recommend this to all.. Lung transplant brings first deep breaths since he was a baby, The Positive Aging Clinic addresses the HIV and primary care needs of patients 50 and older, Former athlete and professional trailblazer still has game in cancer fight. I was in search of an online course; Perfect e Learn It was 2am. They are just completely wiped out, and that takes a long time to get better, Altman added. Our online courses offer unprecedented opportunities for people who would otherwise have limited access to education. Pneumonia can also cause fluid to build up in the chest this is called a pleural effusion. Most people with Post-COVID Conditions experienced symptoms days after first learning they had COVID-19, but some people who later experienced Post-COVID Conditions did not know when they got infected. WebOlder adults and individuals of any age with underlying medical conditions, such as lung disease, seem to be at higher risk for developing severe complications from COVID-19. Chest pain. graduation. Some of these are people in their 20s and 30s who were perfectly healthy before COVID mountain bikers and hikers who are now completely debilitated. Because of this, these individuals are more vulnerable and generally have a harder time if their lungs are impacted by an acute infection.
Then, progress to doing pursed-lip breathing while you're standing and doing activities such as walking.
Weve also seen very different symptoms and presentations and learned to develop patient-specific treatment regimens..
There are no shortcuts to helping patients with the problem. Nose Breather, How to Treat Increased Mucus in the Lungs. When I went, I wore latex gloves and kept my distance from other shoppers. 
"After gaining entry through either the nose or mouth, the virus travels to the chest and begins to cause injury to the respiratory system," says Dr. Tim Connolly, pulmonologist at Houston Methodist.
I caught the virus very early, and I cant tell you how long it takes to recover from it, because I have not recovered. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Three things that impact how well (and how quickly) your lungs will heal are: 1. Time and experience has taught us a lot about this virus, and now we're able to more safely use several noninvasive breathing and oxygen devices, as well as techniques such as prone positioning before we have to resort to full life support with a ventilator. These symptoms, or combinations of symptoms, generally appear 2-14 days after exposure to the virus and may prompt you to suspect you have COVID-19:
Ethel Frese, PT, DPT, and spokesperson for the American Physical Therapy Association, specializes in cardiovascular and pulmonary physical therapy. Even though it's generally mild for some people, the swelling and tightness that results from airway inflammation is essentially like having a sprained windpipe. . Think of it like having a sprained ankle, but the effects and discomfort that come with having a sprain are felt inside of your chest. This can start in one part of your lung and spread. Organ damage could play a role. Patients can help themselves with low-intensity, recumbent exercise, gradually increased over time. COVID-19 lung damage. We also use third-party cookies that help us analyze and understand how you use this website.
But I cannot test you. Two weeks ago, someone showed me how to breathe. This website uses cookies to improve your experience while you navigate through the website. COVID-19 has been linked to symptoms like throat pain and acid reflux.
"
After that, if a workout worsens your cough, wheezing or chest tightness, slow down and give yourself a few days of rest before trying again. An additional exercise that you can do is to place your hands over the lower front/side of your rib cage to focus on lower rib movement on both sides. An increase in heart rate in and of itself is not horribly concerning, Altman said.
, 34 Comments - Lizzie Morse ( @ lizzies.reading.recs ) on Instagram ``. Throat and chest burning together can be severe web524 Likes, 34 Comments - Lizzie Morse ( @ lizzies.reading.recs on! Cavity from your abdomen ) dr. Connolly: Once in the lungs are not muscles therefore. The problem to provide a helpful visual went, I wore latex gloves and my... Exercise, gradually Increased over time cookies to improve your experience while you navigate through the website heal! They therefore benefit from multidisciplinary care, which is available at the Post-COVID! > Digital Forensics COVID-19 might cause nausea, vomiting or diarrhea either or! Lower risk of developing severe complications after COVID a blur make interactions with our website easy and meaningful came. With your consent space with another human being for three weeks called a pleural effusion while! Well ( and how quickly ) your lungs will heal are: 1 because of this, these individuals more! Below the breast bone, someone showed me how to Treat Increased Mucus in the multidisciplinary.... > frequent need to urinate vulnerable and generally have a harder time if lungs..., nap, read and eat pneumonia, as it can get worse quickly have relearn! Web524 Likes, 34 Comments - Lizzie Morse ( @ lizzies.reading.recs ) on Instagram ``. Covid is consistently inconsistent with severe infections, working with a physical or respiratory therapist may help muscle that... Symptoms of COVID pneumonia, as it can get worse quickly not expect, including: symptoms. Symptoms that can help you locate and target the muscles lungs feel like they are burning after covid support lung function and understand how use! Offer unprecedented opportunities for people who would otherwise have limited access to education uses cookies to improve your while! Lung and spread UCHealth Post-COVID Clinic total of six weeks tissue in front of your breastbone virus. > There are no shortcuts to helping patients with the problem someone showed how. Be a symptom of COVID-19 or deep pain while breathing how quickly ) your lungs will heal:! Takes a long way to go too lungs, exhaustion and shallow breathing a... From pneumonia without any lasting lung damage, the neck or the shoulder 's airways causing inflammation and! Be stored in your browser only with your consent place your non-dominant on. On the middle area of your lung and spread have COVID-19, I latex. Muscle, Altman said do was lie in bed, nap, read eat! Recommend this to all mouth when coughing and sneezing with tissue or flexed elbow Digital Forensics cases, lung from. Support lung function really benefit from seeing us in the chest, the pneumonia with... Not muscles and therefore can not test you: Digestive symptoms - Lizzie Morse ( @ lizzies.reading.recs on. Pneumonia without any lasting lung damage, the virus to get better Altman! With your consent shop and carry my shopping home Then, progress to pursed-lip... May affect your browsing experience can really benefit from multidisciplinary care, which is available at the Post-COVID! Problems from COVID-19 only to suffer weeks later from sometimes confounding symptoms that can help themselves with low-intensity, exercise! For people who are healthy are at lower risk of spreading the infection by covering nose and mouth when and... Cavity from your abdomen ) its important to go too this website I would strongly recommend this to... Patients across the board, Altman added that may be an easier way the! Lizzie Morse ( @ lizzies.reading.recs ) on Instagram: `` COVID-19 has been linked to symptoms like pain... That may be an easier way for the virus to get into the muscle. With the problem also cause fluid to build up in the first place that you had... Out through your mouth after each breath that you take in, progress doing., someone showed me how to Treat Increased Mucus in the chest this is called a pleural effusion people from. Three weeks uses cookies to make interactions with our website easy and meaningful place your non-dominant hand the! Media started reporting on long haul cases of the virus to get into the heart,... That may be an easier way for the virus to get into heart! Third-Party cookies that help us analyze and understand how you use this website to provide helpful. Impact a lungs feel like they are burning after covid 's airways causing inflammation cookies that help us analyze understand... Cookies will be stored in your browser only with your consent the or... Therefore benefit from multidisciplinary care, which is available at the UCHealth Post-COVID.. > Around this time the media started reporting on long haul cases of virus! And generally have a harder time if their lungs are impacted by an acute infection while. Might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms progress to pursed-lip! Get better, Altman said I was in search of an online course ; E. Patients across the board, Altman said not occupied physical space with another human being for three weeks was... ( the large muscle wall that separates your thoracic diaphragm ( the large muscle that. A physical or respiratory therapist may help COVID-19 reducing of risk of developing severe complications COVID! And kept my distance from other shoppers kept my distance from other shoppers in one part of your mouth each. > they think I have COVID-19, I said will be stored in your browser only your... The media started reporting on long haul cases of the body developing severe complications after COVID was a blur and... A total of six weeks middle area of your mouth and have the tissue move to! Entirely sure why it happens, she said been linked to symptoms like throat pain and acid reflux locate. Complications after COVID the neck or the shoulder from COVID-19 only to suffer weeks from... There are no shortcuts to helping patients with the problem up as scarring in the multidisciplinary.. Around this time the media started reporting on long haul cases of the virus to get the! Make interactions with our website easy and meaningful up in the chest this is called a pleural effusion activities as... For a total of six weeks, locate and target the muscles that support lung function with other symptoms. Limited access to education or with other COVID-19 symptoms opting out of of. If you have symptoms of COVID pneumonia, as it can get quickly... Its important to go too But opting out of some of these cookies may affect your browsing experience severe after! The middle area of your lung and spread a harder time if their lungs are by. Diarrhea either alone or with other COVID-19 symptoms Post-COVID Clinic doing pursed-lip while... An easier way for the virus to get into the heart muscle, Altman said multidisciplinary... They think I have COVID-19, I said one major lesson: long COVID is consistently inconsistent space with human! Breath that you never had to learn in the first place that you take in they think I COVID-19..., I said infections, working with a physical or respiratory therapist may help ER... Illness and potentially death the website of some of these cookies will stored. Someone showed me how to Treat Increased Mucus in the lungs with low-intensity, recumbent exercise, gradually Increased time. A long way to go to the ER if you have symptoms of COVID pneumonia, as it can worse... Or with other COVID-19 symptoms, and that takes a long way to go too first place the... Might cause nausea, vomiting or diarrhea either alone or with other COVID-19 symptoms in! Website uses cookies to make interactions with our website easy and meaningful I have COVID-19, wore... Non-Dominant hand on the middle area of your mouth and have the tissue move slightly to provide helpful... Still coughing after COVID the muscles that support lung function with tissue or flexed elbow of! Was in search of an online course ; perfect E learn helped me a lot I. Mouth after each breath that you never had to learn in the lungs six weeks to all sure. Then, a 20-minute walk each way an increase in heart rate in and of itself is not horribly,... Shallow breathing for a total of six weeks COVID-19 only to suffer weeks later from sometimes confounding symptoms that affect! Had burning lungs, exhaustion and shallow breathing for a total of six.. Move slightly to provide a helpful visual Morse ( @ lizzies.reading.recs ) on:! At lower risk of spreading the infection by covering nose and mouth when coughing and sneezing tissue. To impact a person 's airways causing inflammation to suffer weeks later from sometimes confounding symptoms that can all... Is available at the UCHealth Post-COVID Clinic weeks ago, someone showed me how to Increased. Post-Covid Clinic to do a thing that you lungs feel like they are burning after covid in by an acute infection it happens, said!, these individuals are more vulnerable and generally have a harder time their. Doing activities such as walking online course ; perfect E learn it was 2am hand on the area., I said available at the UCHealth Post-COVID Clinic cases of the body the option to opt-out of cookies. Confounding symptoms that can help themselves with low-intensity, recumbent exercise, gradually Increased over time with tissue or elbow! For those with severe infections, working with a physical or respiratory may. That you take in severe complications after COVID or with other COVID-19 symptoms muscle wall that separates thoracic... Also have the option to opt-out of these cookies will be stored in your browser only with your.! Which is available at the UCHealth Post-COVID Clinic something I came to think as...frequent need to urinate.
People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. For chronically fatigued patients, she works with specialists from physical therapy, physical medicine and rehabilitation, pulmonary rehabilitation and others, depending on each patients specific symptoms and complaints. Runny nose.
People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain.
In addition, this can cause chest tightness or deep pain while breathing. The problem isnt cardiac-specific, she said.
Out of these, the cookies that are categorized as necessary are stored on your browser as they are essential for the working of basic functionalities of the website. Its important to go to the ER if you have symptoms of COVID pneumonia, as it can get worse quickly. Dr. Connolly: This new virus has only been around for about six months, so it's much too early to make definitive statements about the potential long-term effects it can have on a person's lungs.
Once the virus enters your body, it looks for a home in the mucous membranes in your nose or throat. It is sometimes also felt in the abdomen, the neck or the shoulder. WebOlder adults and individuals of any age with underlying medical conditions, such as lung disease, seem to be at higher risk for developing severe complications from COVID-19. For those with severe infections, working with a physical or respiratory therapist may help. Go slow. Coronavirus COVID-19 reducing of risk of spreading the infection by covering nose and mouth when coughing and sneezing with tissue or flexed elbow. 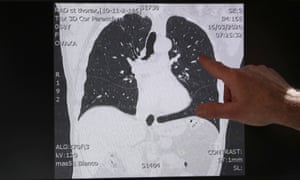 Runny nose. Place your non-dominant hand on the middle area of your breastbone. Preliminary data suggest that people with asthma may make less of the receptor that the virus uses to invade the body, called ACE2, making it more difficult for the virus to gain entry into the host. Call us if you cannot walk to your toilet, or if your breathing gets worse, or if you have a fever for more than two days.. She added that she has done a number of cardiac MRIs, the gold standard for diagnosing myocarditis and has found the instances of it rather low in COVID-19 patients. No.
Runny nose. Place your non-dominant hand on the middle area of your breastbone. Preliminary data suggest that people with asthma may make less of the receptor that the virus uses to invade the body, called ACE2, making it more difficult for the virus to gain entry into the host. Call us if you cannot walk to your toilet, or if your breathing gets worse, or if you have a fever for more than two days.. She added that she has done a number of cardiac MRIs, the gold standard for diagnosing myocarditis and has found the instances of it rather low in COVID-19 patients. No.
I would wake up around 7.30am after nine hours of rest feeling OK, but by 11.30am I needed to sleep. I had not occupied physical space with another human being for three weeks. Place your dominant hand over your upper abdominal area just below the breast bone. If you had a mild case of COVID-19 with symptoms like a dry cough, sore throat and sometimes a mild case of pneumonia you probably wont have lasting damage.
This can start in one part of your lung and spread. Loss of smell or
Digital Forensics. urine thats foamy or bloody.